Understanding Ways To Manage Neuropathy Pain In The Feet
Neuropathy pain in the feet can significantly impact daily life, making simple activities like walking or standing uncomfortable. This condition, often characterized by tingling, burning, or sharp sensations, affects millions of people and can stem from various underlying causes. Understanding effective management strategies is essential for improving comfort and maintaining quality of life.
Living with nerve pain in the feet requires a comprehensive approach that combines medical guidance, lifestyle adjustments, and consistent self-care. While complete elimination of symptoms may not always be possible, many individuals find significant relief through a combination of proven management techniques. This article explores practical strategies and evidence-based approaches to help address this challenging condition.
What Causes Neuropathy Pain in the Feet
Nerve damage in the feet can result from numerous factors, with diabetes being one of the most common culprits. High blood sugar levels over time can damage nerve fibers throughout the body, particularly in the extremities. Other frequent causes include vitamin deficiencies, especially B vitamins, which are crucial for nerve health. Chemotherapy treatments, certain medications, and autoimmune disorders can also trigger nerve damage. Physical injuries, infections, and exposure to toxins may contribute to the development of symptoms. Alcohol abuse represents another significant risk factor, as excessive consumption can lead to nutritional deficiencies and direct nerve damage. Hereditary conditions and chronic kidney disease round out the list of potential causes. Identifying the underlying cause with a healthcare professional is crucial for developing an effective management plan tailored to individual circumstances.
Medical Treatment Approaches for Foot Nerve Pain
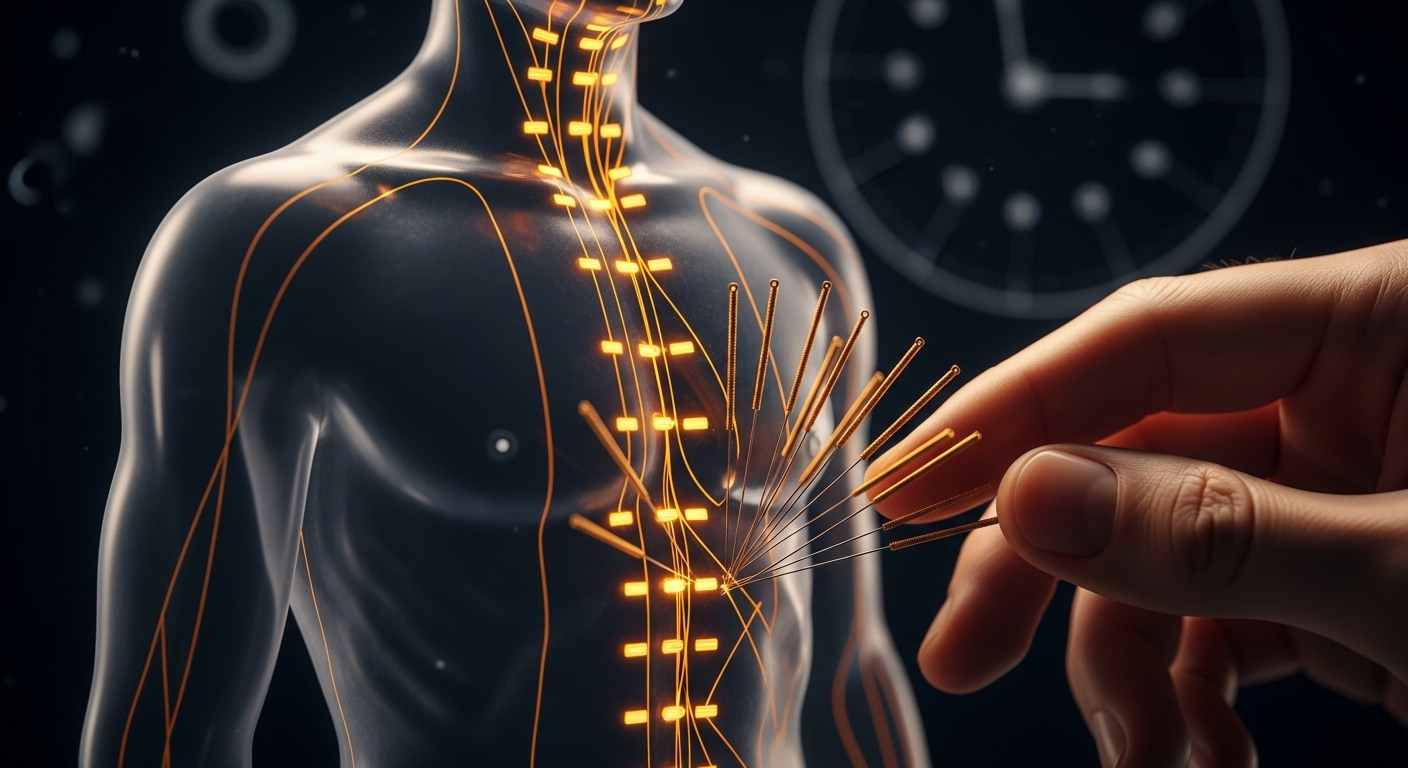
Healthcare providers typically recommend several treatment options depending on the severity and cause of symptoms. Prescription medications often form the first line of defense, including anticonvulsants originally developed for seizure disorders but effective for nerve pain. Antidepressants, particularly tricyclics and serotonin-norepinephrine reuptake inhibitors, can help modulate pain signals. Topical treatments containing capsaicin or lidocaine provide localized relief without systemic side effects. Physical therapy offers exercises designed to improve strength, balance, and circulation in affected areas. Transcutaneous electrical nerve stimulation (TENS) units deliver gentle electrical impulses that may interrupt pain signals. In cases where specific vitamin deficiencies are identified, supplementation under medical supervision can address the root cause. For diabetic nerve pain, maintaining optimal blood sugar control remains paramount. Some individuals benefit from alternative therapies such as acupuncture, though results vary. Regular monitoring and adjustment of treatment plans ensure the most effective symptom management over time.
Lifestyle and Daily Care Tips For Neuropathy Pain In The Feet
Daily habits play a crucial role in managing symptoms and preventing further nerve damage. Proper foot care begins with daily inspections for cuts, blisters, or areas of redness that might go unnoticed due to reduced sensation. Washing feet with lukewarm water and mild soap, followed by thorough drying, especially between toes, prevents infections. Moisturizing dry skin while avoiding the areas between toes helps maintain skin integrity. Wearing properly fitted shoes with adequate cushioning protects feet from injury and pressure points. Seamless socks made from breathable materials reduce friction and irritation. Regular exercise, particularly low-impact activities like swimming or cycling, improves circulation and overall nerve health. Maintaining a healthy weight reduces pressure on feet and helps control underlying conditions like diabetes. Avoiding prolonged sitting or standing in one position promotes better blood flow. Limiting alcohol consumption and avoiding tobacco use are essential, as both can worsen nerve damage. Creating a safe home environment by removing tripping hazards and using adequate lighting prevents falls and injuries.
Nutritional Support for Nerve Health
Diet plays a fundamental role in supporting nerve function and potentially slowing progression of symptoms. A balanced diet rich in B vitamins, particularly B1, B6, and B12, supports nerve repair and function. Foods like whole grains, lean meats, fish, eggs, and leafy greens provide these essential nutrients. Antioxidant-rich fruits and vegetables combat oxidative stress that can damage nerves. Omega-3 fatty acids found in fatty fish, walnuts, and flaxseeds have anti-inflammatory properties beneficial for nerve health. Limiting refined sugars and processed foods helps maintain stable blood sugar levels, particularly important for those with diabetes. Adequate hydration supports overall bodily functions, including nerve health. Some individuals find relief through anti-inflammatory eating patterns like the Mediterranean diet. Magnesium-rich foods such as nuts, seeds, and legumes may help reduce muscle cramps and discomfort. Consulting with a registered dietitian can help develop a personalized nutrition plan that addresses specific needs and underlying conditions contributing to nerve pain.
Ways To Manage Neuropathy Pain In The Feet Through Self-Care Techniques
Several self-care strategies can complement medical treatments and provide additional relief. Warm baths or foot soaks can temporarily ease discomfort, though water temperature should be tested carefully due to reduced sensation. Gentle massage of the feet and lower legs promotes circulation and may reduce pain intensity. Elevating feet when sitting or lying down reduces swelling and improves blood flow. Practicing stress-reduction techniques like meditation, deep breathing, or yoga can help manage pain perception and improve overall well-being. Using orthotic inserts or custom shoe modifications provides additional support and cushioning. Alternating between rest and activity prevents overexertion while maintaining mobility. Some individuals find relief through contrast therapy, alternating between warm and cool compresses. Maintaining a consistent sleep schedule and creating a comfortable sleep environment helps manage pain that often worsens at night. Keeping a symptom diary helps identify triggers and patterns, enabling better communication with healthcare providers. Support groups, whether in-person or online, offer emotional support and practical tips from others experiencing similar challenges.
When to Seek Professional Medical Guidance
Recognizing when symptoms require professional evaluation is essential for preventing complications and optimizing treatment. New or suddenly worsening symptoms warrant immediate medical attention, as they may indicate progression of underlying conditions. Signs of infection such as redness, warmth, swelling, or discharge from foot wounds require prompt care. Changes in skin color or temperature in the feet could signal circulation problems. Difficulty walking or maintaining balance increases fall risk and needs assessment. Symptoms that significantly interfere with daily activities or sleep quality deserve professional intervention. If current management strategies stop providing relief, treatment adjustments may be necessary. Regular follow-up appointments allow healthcare providers to monitor condition progression and modify treatment plans accordingly. Individuals with diabetes should maintain consistent podiatry visits to prevent serious complications. Open communication with healthcare teams ensures comprehensive care addressing both symptoms and underlying causes.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Managing nerve pain in the feet requires patience, persistence, and a multifaceted approach. While the condition can be challenging, many individuals achieve meaningful symptom relief through a combination of medical treatment, lifestyle modifications, and consistent self-care. Working closely with healthcare providers to develop and adjust personalized management plans offers the best opportunity for improved comfort and quality of life. Each person’s experience is unique, and what works for one individual may differ for another, making ongoing communication with medical professionals essential for optimal outcomes.




